
An information session for students interested in enrolling in BA685: Healthcare Delivery in Emerging Markets will be held at 5:30 p.m. on Monday, Oct. 28 at the Ross School of Business, Blau Hall Room 1210. The class is offered by Michigan Ross and is organized and primarily funded by WDI.
The class is comprised mostly of second-year MBA students, but is open to all graduate students. It provides students with on-the-ground experience in a foreign country while also contributing to the success of partner health clinics and hospitals. The class also is designed to increase participants’ international leadership capabilities and enhance their awareness of diverse business issues within the current global landscape. It is taught by WDI President Paul Clyde.
The course responds to the increasing need from future employers that managers have international business perspectives to augment their business and management knowledge. During the first part of the term, students learn about healthcare in emerging markets through lectures, guest speakers and case discussions. Students are then divided into five teams and prepared for visits to their selected country, traveling to those destinations in late February and early March.
Last year, student teams worked in Ethiopia, India, Kenya, Peru and Rwanda.
Kisii Eye Hospital in Kisii, Kenya plans to improve operations so that it can grow to 5,000 surgeries per year, later reaching 10,000 surgeries per year. Recommendations on operations, organization and revenue generation were developed, some of which are being implemented over the coming months. We are also helping them develop a business plan to be used with potential investors.
Studying for her master’s degree in public health, Alison Granger was interested in a course at the University of Michigan that would let her take the lessons from her textbooks and classroom lectures and put it into practice.
That’s why she enrolled in BA685: Healthcare Delivery in Emerging Markets, a course offered at the Ross School of Business.
“I was interested in getting a more in-the-field, global perspective on what I’ve learned so far in class,” said Granger, who traveled to Ethiopia for her project. “And I did with this class.”
The class is comprised mostly of MBA2 students, but also is open others pursuing other graduate degrees such as Granger. It’s designed to enhance participants’ international leadership capabilities, increase awareness of diverse business issues within the current global landscape, provide on-the-ground experience in a foreign country and contribute to the success of partner health clinics and hospitals. It is taught by WDI President Paul Clyde.
The course, organized and primarily funded by WDI with some financial support from Michigan Ross, responds to the increasing need for managers with international business perspectives to augment their business and management knowledge. During the first part of the term, students learned about healthcare in emerging markets through lectures, guest speakers and case discussions. Students were then divided into five teams and prepared for visits to their selected country, traveling to those destinations in late February and early March.
This year, student teams worked in Ethiopia, India, Kenya, Peru and Rwanda. All five teams presented recaps of their projects on April 22 at Michigan Ross.
Clyde said the travel-study course lets students combine what they learned in the classroom with hands-on experience in the field. It features a collaborative learning environment with faculty and students learning from each other in an action-based learning setting.
“Through this course teams of students from Ross, SPH and School of Information have provided our partner healthcare organizations value through analysis of their operations, customers and strategy,” Clyde said. “Through this experience, the students gain unusual insights into the opportunities and challenges of operating healthcare organizations in LMICs.”
Here is a recap of the BA685 projects:
More than 1 million infants die each year due to severe respiratory distress, with 99 percent of these deaths in low- to middle-income countries, according to the World Health Organization. Current noninvasive ventilators are expensive, require skilled operators, and fail during power outages that are common in emerging markets. AIM Tech developed NeoVent, a low-cost, low-tech, easy-to-use ventilator that is non-electric and has only one moving part. It also can be manufactured at scale for less than 1 percent the cost of conventional ventilators.
 AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
Mumbai and Chennai, and interviewed and provided product demonstrations to 24 healthcare facilities, one government official, two manufacturers and one distributor. The students found that the Indian healthcare market shows a high-growth trajectory. The government’s focus on entrepreneurship, insurance, and neonatology also creates favorable climate and demand for NeoVent, while clinicians see the product as unique, necessary and value it at a higher-than-planned price, the students noted.
They recommended AIM Tech license NeoVent to a multinational corporation with an existing foothold in the Indian market. Another suggestion was to pilot NeoVent with a large hospital following FDA approval.
 The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
Based on research and interviews with hospitals with its own medical gas plants on-site, the students’ findings showed that EADG would benefit from building its own facility and could learn from other hospitals that have done the same. On the question of whether to sell excess medical gas, the students’ research showed it would not be a good decision to do so. It is not profitable, the research found, and there is robust competition and several barriers to entry in the market. The students encouraged EADG to begin the bidding process soon to select equipment suppliers because the hospital is expected to open in 2021. They also suggested EADG monitor the medical gas market for any movement or changes in government policy that might make it more profitable to sell excess medical gas.
Timely and accurate data reports are vital to operations at rural health clinics. Electronic records have been implemented, but poor staffing and internet connection have made e-records ineffective. The Ihangane Project, in partnership with nurses from rural health centers, created E-Heza Digital Health Record to deliver more timely and accurate data to the Rwanda Ministry of Health. The ministry has requested that E-Heza be expanded throughout Rwanda to serve maternal child care.
 The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The students recommended a framework that evaluated efficiency in terms of timeliness, cost savings and data quality.
For next steps, the students recommended recording observational data for each process in the workflow, testing the framework for E-Heza and other health modules and exploring and quantifying the potential adverse effect due to poor data quality.
The Kisii Eye Care Institute started in 2013 and it has grown from an eye care service provider to a medical eye hospital and training center. It provides 3,000 surgeries annually but wants to increase the demand and capacity to 5,000 per year. Kisii operates as a social enterprise using an entrepreneurial approach to solve a social problem – avoidable blindness and visual impairment. Services are provided at normal rates for those who can afford them and substantially below cost to low-income members of their community.
 The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
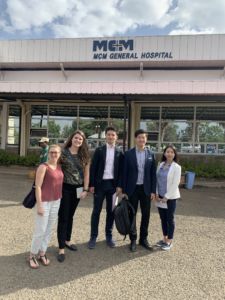
PAMS Policlinico wants to become a gastrointestinal (GI) center of excellence. It currently offers GI services and recently a GI doctor from the University of Michigan visited to develop an operational understanding.
 Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
The students’ research and on-site observations and interviews showed: A lack of standardized practices lead to operational inefficiencies and lowered capacity even with sufficient personnel; contract incentives are not structured to achieve best outcome for PAMS; omission of certain accounting practice lowers visibility into financial health of PAMS and each specialties; and, the Polyclinic is one of the few providers of colonoscopies in the region.
The student team’s recommendations included: optimizing processes allowing for maximizing use of resources, including supplies and the time of healthcare providers; standardizing processes also decreases waste and allows more patients to be treated per week, ultimately increasing patient volume and with it, revenue.
In sub-Saharan Africa, the private sector provides family planning solutions to almost 40 percent of women. But that isn’t the case in Malawi, a country that’s long been dominated by donor-funded commodities. Erika Beidelman and Andrea Bare at the William Davidson Institute explore Malawi’s family planning landscape, highlighting five factors that may be limiting the private sector’s involvement – issues that may apply to other countries with histories of donor-funded healthcare.
WDI reviewed and documented lessons learned by the Global Alliance for Clean Cookstoves (the Alliance) since its inception. The Alliance is a public-private partnership hosted by the United Nations Foundation that aims to save lives, improve livelihoods, empower women, and protect the environment by creating an efficient and thriving global market for clean and efficient household cooking solutions. The alliance’s goal is to facilitate the creation of a market that enables 100 million households in developing countries to access clean cooking solutions by 2020. Through interviews with staff and alliance partners in Washington, D.C., Kenya and Bangladesh, WDI sought to identify which of the alliance’s efforts focused on building the market for clean cooking solutions have worked, which of these efforts have been less successful, and how these outcomes might be translated into lessons learned and strategic options for the alliance. WDI also sought to develop insights that could be beneficial for other organizations interested in a global approach to market creation in low income settings. This work also resulted in the development of a conceptual framework for how to accelerate impact industries, which was the subject of an article published online by The Stanford Social Innovation Review in June 2018.
Stanford Social Innovation Review article.
Colm Fay will participate in a panel discussion hosted by the Alliance at SOCAP 2018
WDI is studying how the availability of grants and technical assistance facilitates the efforts of health enterprises to reach scale, particularly in the provision of family planning products and services. This study tracks the performance of a subset of participants in the HANSHEP Health Enterprise Fund (HHEF). In the first year of this study, the research team identified a set of key capacities that participating health enterprises considered to be important in achieving increases in access to family planning, and how support from the HHEF helped to build these capacities. In the second year of the study, the team is seeking to better understand the economics of how family planning products and services are integrated into the enterprise’s business model. The team is also exploring other sources and types of support received by these enterprises and any gaps that remained, with the aim of improving the design of similar interventions in the future.
WDI conducted market research for a company that designs and manufactures unmanned aerial vehicles (UAV) to transport small goods. Use of UAVs to transport items in low- and middle-income countries is low but they show significant potential for making healthcare commodities available in settings with poor infrastructure challenges. The purpose of WDI’s market research was to identify opportunities for this company’s expansion into both healthcare and non-healthcare sectors in Kenya, the Philippines, Zambia and non-healthcare sectors in Senegal. Data had been collected from decision-makers in public and private organizations in each country covering several topics such as product use cases, current transport activities and factors influencing the purchase or lease decision. Data was then analyzed and summarized into a go-to-market strategy for this UAV company in these four countries. This project was funded by the Bill & Melinda Gates Foundation.
The William Davidson Institute is a collaborative, multi-disciplinary organization. As a result, WDI often engages multiple sector and services teams in our work. The following project undertaken by both our Healthcare sector and Performance Measurement and Improvement service demonstrates our holistic approach.
WDI is working with global medical device company, Becton, Dickinson & Company (BD), to assess the impact of the new program, Infection Prevention and Control, in Kenya. The goal of the program is to strengthen health worker and patient safety through appropriate safe intravenous infusion therapy practices, leveraging BD’s longstanding knowledge and safety-engineered technology designed to reduce the rate of needle-stick injuries in HCWs, thus contributing to the prevention of injection-transmitted infections such as HIV and other blood-borne pathogen transmission.
The William Davidson Institute is a collaborative, multi-disciplinary organization. As a result, WDI often engages multiple sector and services teams in our work. The following project undertaken by both our Healthcare sector and Performance Measurement and Improvement service demonstrates our holistic approach.
The goal of the program is to support quality laboratory systems, which are needed in order to effectively scale-up HIV prevention, care and treatment efforts. WDI’s work includes developing the Monitoring and Evaluation design and implementation plan, and collecting data to measure the impact of the program activities that include Strengthening Laboratory Management Towards Accreditation (SLMTA) training and BD mentorship, in multiple labs across Kenya, Uganda, Rwanda and India.

WDI has been commissioned by Becton, Dickinson and Company (BD), one of the largest global medical technology companies in the world, to be a monitoring and evaluation partner for their BD-PEPFAR public-private partnership with the U.S. State Department’s Office of the Global AIDS Coordinator (OGAC) and the U.S. Centers of Disease Control and Prevention (CDC). The U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) is the largest commitment by any nation to combat a single disease in history.
As part of this work, Heather Esper, WDI’s senior program manager for the Performance Measurement Initiative (PMI), was invited to participate in a series of meetings with partners working on two BD-PEPFAR programs – Labs for Life and Infection Prevention and Control.
PMI, along with WDI’s Healthcare Initiative, is developing and will conduct an assessment of Phase 3 of the third Labs for Life partnership. The Institute will explore the impact and cost effectiveness of the Labs for Life activities, including laboratory system strengthening for improving quality management practices and fortifying specimen referral systems for HIV and TB.
WDI also conducted a retrospective assessment of the impact of selected activities for Phase 2 of Labs for Life. This work included a quantitative and qualitative analysis of a Kenya lab’s accreditation, and a quantitative assessment of the Kenyan National Public Health Laboratory Center of Excellence for Equipment Calibration, Certification and Training, which was set up and initiated by BD in partnership with the Ministry of Health. Esper and Pascale Leroueil, vice president of WDI’s Healthcare Initiative, presented the findings in April 2018 at the Labs for Life Phase 3 kickoff in London.

Deborah Birx, Ambassador-at-Large, U.S. Global AIDS Coordinator & U.S. Special Representative for Global Health Diplomacy
Also in conjunction with PEPFAR and BD, OGAC and the CDC, the Institute is working to design and implement an assessment of the impact of a new program, Infection Prevention and Control, in Kenya. The goal of the program is to strengthen health worker and patient safety through appropriate safe intravenous infusion therapy practices, leveraging BD’s longstanding knowledge and safety-engineered technology for averting HIV, hepatitis and other blood-borne pathogen transmission.
Esper said WDI is proud to be developing and implementing strong monitoring and evaluation systems on two PEPFAR public-private partnerships with BD, the Office of the Global AIDS Coordinator and the Centers for Disease Control and Prevention focused on the prevention and diagnosis of HIV/AIDS.
“Both of these monitoring, evaluation, research and learning (MERL) systems have a large focus on cost-effectiveness and will help inform activities that should be scaled to help meet the UNAIDS’ treatment goals and beyond,” she said. “These systems also allow partners to track activities as they are implemented with the goal of delivering more impact.”
As part of this work, on July 11 Esper and WDI Healthcare Research Associate Erika Beidelman, traveled to New York for two working meetings related to the monitoring and evaluation design of both PEPFAR programs.
That same morning, BD, PEPFAR and other BD guests rang the NYSE Opening Bell to celebrate a decade of partnerships to address HIV/AIDS as well as to recognize PEPFAR’s 15 year anniversary, which has impacted 14 million men, women, and children with HIV & AIDS globally. Deborah Birx, Ambassador-at-Large, U.S. Global AIDS Coordinator & U.S. Special Representative for Global Health Diplomacy, Office of Global AIDS Coordinator, was recognized by BD for her leadership.