International Clinical Laboratories (ICL) and its partners have been approached by the Ethiopian government to develop a business that would safely dispose of medical waste for healthcare facilities across Ethiopia. Through a series of projects, WDI has worked with ICL to develop a business and operations plan for biomedical waste that includes financials and an in-depth analysis of the various training requirements, operations complexities and expected costs. In 2020, ICL found a sponsor for autoclave machines and reached out to WDI to provide revised financials for purposes of investment.
In 2019, Awash Bank in partnership with WDI explored the development of a program that leveraged remittances as both collateral for the loan and information about the borrower. By allowing the borrower to develop a credit rating, remittances can increase access to capital for SMEs at a reasonable rate. In 2020, Awash Bank formally created the loan product and published a procedure manual. Efforts are underway to market this loan product in Ethiopia and with the diaspora community in the US.
Due diligence was conducted on five SMEs for investment readiness for the Infra Group, a to-be-launched private equity fund that aspires to invest in Ethiopian SMEs using hard currency. A due diligence checklist was also developed that can be used by anyone conducting due diligence on SMEs.
Studying for her master’s degree in public health, Alison Granger was interested in a course at the University of Michigan that would let her take the lessons from her textbooks and classroom lectures and put it into practice.
That’s why she enrolled in BA685: Healthcare Delivery in Emerging Markets, a course offered at the Ross School of Business.
“I was interested in getting a more in-the-field, global perspective on what I’ve learned so far in class,” said Granger, who traveled to Ethiopia for her project. “And I did with this class.”
The class is comprised mostly of MBA2 students, but also is open others pursuing other graduate degrees such as Granger. It’s designed to enhance participants’ international leadership capabilities, increase awareness of diverse business issues within the current global landscape, provide on-the-ground experience in a foreign country and contribute to the success of partner health clinics and hospitals. It is taught by WDI President Paul Clyde.
The course, organized and primarily funded by WDI with some financial support from Michigan Ross, responds to the increasing need for managers with international business perspectives to augment their business and management knowledge. During the first part of the term, students learned about healthcare in emerging markets through lectures, guest speakers and case discussions. Students were then divided into five teams and prepared for visits to their selected country, traveling to those destinations in late February and early March.
This year, student teams worked in Ethiopia, India, Kenya, Peru and Rwanda. All five teams presented recaps of their projects on April 22 at Michigan Ross.
Clyde said the travel-study course lets students combine what they learned in the classroom with hands-on experience in the field. It features a collaborative learning environment with faculty and students learning from each other in an action-based learning setting.
“Through this course teams of students from Ross, SPH and School of Information have provided our partner healthcare organizations value through analysis of their operations, customers and strategy,” Clyde said. “Through this experience, the students gain unusual insights into the opportunities and challenges of operating healthcare organizations in LMICs.”
Here is a recap of the BA685 projects:
More than 1 million infants die each year due to severe respiratory distress, with 99 percent of these deaths in low- to middle-income countries, according to the World Health Organization. Current noninvasive ventilators are expensive, require skilled operators, and fail during power outages that are common in emerging markets. AIM Tech developed NeoVent, a low-cost, low-tech, easy-to-use ventilator that is non-electric and has only one moving part. It also can be manufactured at scale for less than 1 percent the cost of conventional ventilators.
 AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
Mumbai and Chennai, and interviewed and provided product demonstrations to 24 healthcare facilities, one government official, two manufacturers and one distributor. The students found that the Indian healthcare market shows a high-growth trajectory. The government’s focus on entrepreneurship, insurance, and neonatology also creates favorable climate and demand for NeoVent, while clinicians see the product as unique, necessary and value it at a higher-than-planned price, the students noted.
They recommended AIM Tech license NeoVent to a multinational corporation with an existing foothold in the Indian market. Another suggestion was to pilot NeoVent with a large hospital following FDA approval.
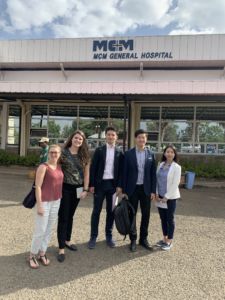 The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
Based on research and interviews with hospitals with its own medical gas plants on-site, the students’ findings showed that EADG would benefit from building its own facility and could learn from other hospitals that have done the same. On the question of whether to sell excess medical gas, the students’ research showed it would not be a good decision to do so. It is not profitable, the research found, and there is robust competition and several barriers to entry in the market. The students encouraged EADG to begin the bidding process soon to select equipment suppliers because the hospital is expected to open in 2021. They also suggested EADG monitor the medical gas market for any movement or changes in government policy that might make it more profitable to sell excess medical gas.
Timely and accurate data reports are vital to operations at rural health clinics. Electronic records have been implemented, but poor staffing and internet connection have made e-records ineffective. The Ihangane Project, in partnership with nurses from rural health centers, created E-Heza Digital Health Record to deliver more timely and accurate data to the Rwanda Ministry of Health. The ministry has requested that E-Heza be expanded throughout Rwanda to serve maternal child care.
 The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The students recommended a framework that evaluated efficiency in terms of timeliness, cost savings and data quality.
For next steps, the students recommended recording observational data for each process in the workflow, testing the framework for E-Heza and other health modules and exploring and quantifying the potential adverse effect due to poor data quality.
The Kisii Eye Care Institute started in 2013 and it has grown from an eye care service provider to a medical eye hospital and training center. It provides 3,000 surgeries annually but wants to increase the demand and capacity to 5,000 per year. Kisii operates as a social enterprise using an entrepreneurial approach to solve a social problem – avoidable blindness and visual impairment. Services are provided at normal rates for those who can afford them and substantially below cost to low-income members of their community.
 The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
PAMS Policlinico wants to become a gastrointestinal (GI) center of excellence. It currently offers GI services and recently a GI doctor from the University of Michigan visited to develop an operational understanding.
 Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
The students’ research and on-site observations and interviews showed: A lack of standardized practices lead to operational inefficiencies and lowered capacity even with sufficient personnel; contract incentives are not structured to achieve best outcome for PAMS; omission of certain accounting practice lowers visibility into financial health of PAMS and each specialties; and, the Polyclinic is one of the few providers of colonoscopies in the region.
The student team’s recommendations included: optimizing processes allowing for maximizing use of resources, including supplies and the time of healthcare providers; standardizing processes also decreases waste and allows more patients to be treated per week, ultimately increasing patient volume and with it, revenue.

A 2018 WDI MAP team in Ghana.
Carrie Boyle, a MBA student at Michigan’s Ross School of Business, hopes to work in philanthropy somewhere in the U.S. after graduation. But for a couple of weeks in March, she is excited to be traveling to India as part of the school’s annual Multidisciplinary Action Projects (MAP).
“Working in another country is something I may never get the chance to do again,” she said. “This will be my first time in India and the country really interests me.”
Boyle and her teammates will work with Michigan Academy for the Development of Entrepreneurs (MADE), a nonprofit institute established at Ross by the Zell Lurie Institute for Entrepreneurial Studies, in partnership with WDI and Aparajitha Foundations. MADE works with entrepreneurship development organizations in India to help entrepreneurs operating small- and medium-sized enterprises (SMEs) succeed.
Boyle said she had some criteria when looking for MAPs that interested her.
“I wanted an opportunity to be on the ground having meaningful conversations with the people most immediately impacted by SMEs,” she said. “SMEs employ so many people and impact so many lives.”
Her teammate Shoko Wadano said she too is interested in working with SMEs, “which are very common in India.”
“I’m interested in how businesses mature in India,” she said. “I want to learn what pressures and impacts SMEs have in common, and what kind of value we can bring to them.”
WDI is sponsoring the MADE MAP project along with 10 others this year. MAP is an action-based learning course in which MBA students receive guidance from faculty advisors from WDI and Ross. Each project requires analytical rigor, critical thinking and teamwork. (Find out more about WDI’s MAP projects over the years here.)
After learning about their projects and conducting secondary research for several weeks, the student teams spend two to four weeks working with their organizations in the field.

David Butz
“The complementarities between the talents our students bring and what our sponsors need are sublime,” said David Butz, a WDI senior research fellow in the Healthcare sector who is an advisor on two projects. “Our students experience impact in brand new ways. Our sponsors learn, too, how disciplined management methods can yield dramatic innovations.”
Butz said he enjoys working with the student teams on MAP because it “poses such a unique challenge for both the students and their sponsor organizations, and forces us all to think big.”
“For me, the best achievements are tangible, direct and narrow but at the same time big and high-impact,” he said. “In our short time, can we help to break some key bottleneck, expedite a critical process pathway or otherwise liberate resources and expand capacity? Is the innovation scalable or replicable elsewhere? Do the students and organizations thereby feel empowered?”
Here is a summary of each WDI-sponsored MAP project:
Aravind Eye Care System – India
MAP Team: Rohan Dash, Sid Mahajan, Aman Rangan, Nik Royce
Aravind Eye Care System (AECS) is a vast network of hospitals, clinics, community outreach efforts, factories, and research and training institutes in south India that has treated more than 32 million patients and has performed 4 million surgeries since its 1976 founding.
AECS opened a tertiary eye care center in Chennai in September 2017 that will ultimately serve more patients than any other facility in the AECS system. The MAP team will formulate a detailed three-year strategic plan for Aravind Eye Hospital in Chennai.
CURE International, Inc. – Kenya, Ethiopia, Zambia, Uganda
MAP Team: Dominique James, Sarah Raney, Hannah Viertel, Olga Vilner Gor
CURE operates clubfoot clinics in 17 countries around the world, each tasked with helping children and families deal with the congenital deformity that twists the foot, making it difficult or impossible to walk.
For CURE, the student team will develop a strategic evaluation framework to assess opportunities for market entry and expansion building on global data.
Ghana Emergency Medicine Collaborative – Ghana
MAP Team: Benjamin Desmond, Benjamin Quam, Nicholas Springmann, Vishnu Suresh
The Ghana Emergency Medicine Collaborative aims to improve emergency medical care in Ghana through innovative and sustainable training programs for physician, nursing and medical students. The goal of the training programs is to increase the number of qualified emergency health care workers retained over time in areas where they are most needed.
The MBA team will formulate a detailed strategy to implement interoperable digital payment systems in Ghanian hospital emergency departments.
India Investment Fund – India
The India Investment Fund is working to become the first international, student-run fund at the Ross School of Business. Ross MBA students would be responsible for investing, managing and growing a real investment portfolio.
MAP Team: Charlie Manzoni, Patrick Riley, Queenie Shan, Sheetal Singh
The student team will conduct due diligence on Indian small- and medium-sized enterprises to assess viability for investments, and an appropriate financing instrument.
Infra Group – Ethiopia
MAP Team: Rin Chou, Chandler Greene, Yuki Ito, Brittany Minor
Infra Group is diversified international group with business units in financial services, industries and infrastructure development. Infra Group helps build a more prosperous society through global-scale business development with integrity as its top priority.
The MAP team will conduct due diligence on a group of small- and medium-sized enterprises (SMEs), and recommend which ones to invest in and what amount to invest.
Lviv Business School & Ukranian Catholic University – Ukraine
MAP Team: Blake Cao, Emily Fletcher, Kelsey Pace, Adam Sitts
Lviv Business School and Ukranian Catholic University is a private educational and research institution in western Ukraine.
The student team will undertake a needs assessment of the small- and medium-sized enterprises (SMEs) to determine if Lviv Business School should begin offering consulting services to these SMEs and if so, how those should be structured.
MADE – Poornatha/Aparajitha Foundations – India
MAP Team: Carrie Boyle, Lawrence Chen, Dillon Cory, Shoko Wadano
Michigan Academy for the Development of Entrepreneurs (MADE) is a nonprofit institute established at the Ross School of Business by the Zell Lurie Institute for Entrepreneurial Studies, in partnership with WDI and Aparajitha Foundations. MADE works with entrepreneurship development organizations in developing countries to give individuals operating businesses in these environments the knowledge and best practices they need to thrive.
The MAP team will develop an expansion plan for MADE in the southern Indian state of Tamil Nadu.
The Ihangane Project – Rwanda
MAP Team: Lauren Baum, Nadia Kapper, Paul Mancheski, Jason Yu
The Ihangane Project (TIP) empowers local communities to develop sustainable, effective, and patient-centered health care delivery systems that holistically respond to the needs of vulnerable populations. Partnering with Ruli District Hospital and its associated health centers, TIP is working to identify key strategies for improving health outcomes.
The student team will develop a business model to grow the ready-to-use therapeutic food that is used to treat severe, acute malnutrition.
WEEKEND MBA MAP PROJECTS
Awash Bank – Ethiopia
MAP Team: Matthew Campbell, Joshua Dodson, Joseph McCarty, Aman Suri
Awash Bank, a private, commercial bank, was established in 1995 and features more than 375 branches across the country.
The MAP team will develop a product that can provide capital to small- and medium-sized enterprises (SMEs) in Ethiopia by utilizing remittances already being sent back to that country. The students will work with the bank on all aspects of the loan product. They also will give the bank recommendations on how to monitor the loan and provide business support to SMEs that borrow from the fund.
Grace Care Center – Sri Lanka
MAP Team: Daniel Cady, Yizhou Jiang, Gerardo Martinez, Daniel Murray
The Grace Care Center (GCC) is a home to about 70 orphaned children that offers daycare services and vocational training. It also is home to several poor and displaced seniors, many of whom have chronic health issues such as hypertension and diabetes.
Past MAP student teams from the Ross School of Business developed a diabetic care center model for GCC. This year’s student team will examine the current model and make any needed updates and revisions.
International Clinical Labs – Ethiopia
MAP Team: Emily Mascarenas, Torre Palermino, Alexander Santini, Matthew Traitses
ICL was established in 2004 to provide quality laboratory service all over Ethiopia. ICL serves more than 240 health care centers throughout the country, and is expanding its service throughout Ethiopia.
The Ethiopian government is building its first medical waste incinerator facility outside the capital city of Addis Ababa and has committed to building seven more around the country. WDI is assisting a group of business managers with business plan advice who are interested in managing the business aspects of operating the incinerators. The MAP team will develop a proposal to be presented to the government later this year for the business managers to operate the incinerators.

Ethiopia’s first medical waste incinerator facility under construction outside Addis Ababa.
A group of business leaders are partnering with the William Davidson Institute to find both financially and ecologically sustainable solutions to Ethiopia’s medical waste problem.
While Ethiopia has official directives that mandate the proper and timely disposal of medical waste, enforcement often has been challenging. This has resulted in warehouses full of expired pharmaceuticals along with biomedical waste generated by hospitals and other healthcare facilities. The Ethiopian government recently decided to address the pharmaceutical waste problem and is looking for a company from the private sector to be part of a Public-Private Partnership (PPP).
The government has started building its first medical waste incinerator facility outside the capital city of Addis Ababa to burn expired pills, and has committed to building seven more around the country. A group of business managers led by Mel Negussie and Tamrat Bekele are interested in managing the business aspects of operating the incinerators and have asked WDI to help them think through the business plan.
Through the work of WDI staff, including Claire Hogikyan, vice president of administration and publishing at WDI, and a team of Weekend MBA students, WDI is developing a proposal to be presented to the government later this year. The proposal will include analysis on several aspects of the incinerator project, including estimating costs, pricing and a plan to scale it. The plan will include an autoclave facility in Addis Ababa that would handle a buildup of biomedical waste from surrounding healthcare facilities, another challenge the Ethiopian government is trying to address.
The idea for an autoclave facility came after Hogikyan traveled to Ethiopia in fall 2018 on a fact-finding mission. At the end of her week-long visit, Hogikyan thought Negussie and his group needed to go in a different direction. While many expired pharmaceuticals can be incinerated, many cannot. For example, medications that are toxic or items such as inhalers that would explode when burned can not be incinerated. Additionally, there are ongoing environmental concerns that accompany incineration.
Most U.S. hospitals, including at the University of Michigan, use an autoclave to properly dispose of expired pharmaceuticals as well as biomedical waste. An autoclave uses heat to disinfect the material and a grinder -similar to a kitchen sink disposal system enlarged and turned on its side. The disinfected and ground material is spit out onto a conveyor belt where a pulverizer breaks down the material further into indistinguishable components. The remaining waste is then dumped into plastic barrels which are shipped to a landfill and buried.
“An autoclave would improve the environment,” Negussie said. “Addis is growing. It is also becoming polluted. Every hospital burning their own medical waste isn’t going to help. An autoclave is a green solution.”

Negussie also is member of Ethio-American Doctors Group (EADG), a group of more than 250 Western-trained clinicians who have committed time and money toward the development of a world-class tertiary care hospital in Addis Ababa. WDI has worked with EADG since 2014 on the governance of the hospital, capital equipment planning, nurse training and a financial model.
When he and his partners began thinking about the incineration project, he reached out to WDI for assistance. He and his partners have operational and project management experience, he said, but needed WDI to strategize with them, to shape a business plan and provide a roadmap to profitability.
“We need someone to help us think through business concepts from capital expenditures, the ownership, the management, the logistics in terms of how it connects,” Negussie said. “What is the proper way of disposing it? What are the other options? Someone to really do the business plan on the business services. That’s not something we can do.”
The businessmen expect to submit proposals to the Ethiopian government this spring to operate the incinerators and also open an autoclave facility. Negussie said he hopes to have an autoclave in the capital city up and running by fall 2019.
WDI President Paul Clyde said the Ethiopian partnership is a great fit for the Institute. He said Negussie and his partner, Tamrat Bekele, are smart businessmen trying to build a model to solve a problem that hasn’t been addressed by a profitable business in the past.
“Working with them to develop something in medical waste gives us a model that we can take to other countries and work with other partners to develop similar businesses,” Clyde said. “Medical waste is an area that hasn’t received the attention it needs in many countries, but we can expect that to change in the coming years as businesses begin to play a more important role in filling that gap.”
WDI worked with CURE-Ethiopia to identify areas of operation that needed improvement, such as procurement and manufacturing of the braces that used to treat clubfoot. The Institute also proposed changes in strategy and operations, including targeted investments, that would allow CURE to treat all patients born with clubfoot in Ethiopia. Since it was founded ten years ago, CURE-Ethiopia has only been able to treat about one quarter of the people born with the clubfoot in the country each year. A WDI team also developed recommendations for expanding the brace manufacturing operation within Ethiopia.
EADG is a group of more than 250 Western-trained clinicians who have committed time and money toward the development of a world-class tertiary care hospital in Addis Ababa. EADG broke ground on the hospital in 2017 year and expects to open in 2020 with 300 beds, 8 operating rooms and an 80-room multi-specialty clinic. WDI has worked with EADG since 2014 on the governance of the hospital, capital equipment planning and a financial model. This year, WDI developed a model to train nurses that meet international standards. The recommendation also includes financial analysis and partnership recommendations.
WDI is studying how the availability of grants and technical assistance facilitates the efforts of health enterprises to reach scale, particularly in the provision of family planning products and services. This study tracks the performance of a subset of participants in the HANSHEP Health Enterprise Fund (HHEF). In the first year of this study, the research team identified a set of key capacities that participating health enterprises considered to be important in achieving increases in access to family planning, and how support from the HHEF helped to build these capacities. In the second year of the study, the team is seeking to better understand the economics of how family planning products and services are integrated into the enterprise’s business model. The team is also exploring other sources and types of support received by these enterprises and any gaps that remained, with the aim of improving the design of similar interventions in the future.
The William Davidson Institute is a collaborative, multi-disciplinary organization. As a result, WDI often engages multiple sector and services teams in our work. The following project undertaken by both our Healthcare sector and Performance Measurement and Improvement service demonstrates our holistic approach.
The goal of the program is to support quality laboratory systems, which are needed in order to effectively scale-up HIV prevention, care and treatment efforts. WDI’s work includes developing the Monitoring and Evaluation design and implementation plan, and collecting data to measure the impact of the program activities that include Strengthening Laboratory Management Towards Accreditation (SLMTA) training and BD mentorship, in multiple labs across Kenya, Uganda, Rwanda and India.