Through the Strengthening Health Outcomes through the Private Sector (SHOPS) Plus USAID-funded project led by Abt Associates, WDI developed a Madagascar Health Enterprise and Innovation Directory based on a mapping activity that identified innovative health enterprises in Madagascar, and the partners and types of support available to them. The directory illustrated the types of financial and technical support available to health enterprises, and the partners that provide various types of support. WDI leveraged the insights gathered through the mapping activity to contribute to the development of recommendations that explore how USAID/Madagascar can promote enterprise innovation, leverage private sector resources, and maximize priority health outcomes through financially sustainable health enterprises.
WDI provided the SHOPS Plus team in Madagascar with technical guidance related to a business plan competition offered in collaboration with Orange Fab, which supports development of new health enterprises that positively affect low-income populations. The WDI team also developed Health Entrepreneurship basic and advanced training curricula for students at Madagascar’s Faculty of Medicine at the University of Antananarivo.
WDI’s Healthcare team conducted a project for the Linked Foundation to inform social enterprise investment in Latin America. The Foundation seeks to identify market-based, impact investment opportunities specific to women’s health in Latin America, based on an integrated assessment of the major unmet needs in combination with identification of high-impact solutions and opportunities to foster the enterprise ecosystem and sustainable women’s health solutions. WDI developed an analytic methodology, conducted a landscaping for Colombia and Peru, and finalized a report including recommendations for development of the health investment ecosystem. The report has been widely disseminated in theLatin America impact investment community. Linked anticipates this work will inform their investment strategy as well as catalyzing additional resources to the most-needed areas in women’s health in Latin America.
Kisii Eye Hospital in Kisii, Kenya plans to improve operations so that it can grow to 5,000 surgeries per year, later reaching 10,000 surgeries per year. Recommendations on operations, organization and revenue generation were developed, some of which are being implemented over the coming months. We are also helping them develop a business plan to be used with potential investors.
As part of the the Sustaining Health Outcomes through the Private Sector (SHOPS) Plus USAID-funded project led by Abt Associates, WDI provided diagnostic and consultative services on revenue generation and operational efficiency for four HIV-focused NGOs in the cities of La Romana and Santo Domingo in the Dominican Republic. These four organizations had historically received a significant portion of their funding from the President’s Emergency Plan for AIDS Relief (PEPFAR) and were preparing for transition to sustainable social enterprise models. WDI’s onsite diagnostic and related technical assistance was highly customized to the business models and needs of the individual organizations. The WDI team developed actionable recommendations for the NGO decision makers on how they could modify their strategies and/or operations to work towards financial sustainability. Return visits were made to assess progress and provide additional assistance to the organizations. WDI also provided consulting services to one of the NGOs, Clinica de Familia, for the development of a sustainable business model for its new dermatology clinic.
Populations in low-and-middle-income countries face a variety of barriers to receiving vaccinations, such as vaccine stockouts, cold chain breakdowns, difficulty traveling to a clinic or a lack of sufficiently trained clinic staff. New vaccine technologies have the potential to reduce or eliminate many of these barriers, but the impact of such reductions on actual immunization rates is not clear.
To address this gap, WDI’s Healthcare Team is developing a model to estimate the change in immunization coverage rates associated with a new vaccine introduction. The model includes six main barriers that can be addressed by new technologies. It first considers the prevalence of these barriers in the target population and then considers how effectively a new technology can address those same barriers. Those two factors are combined to estimate the change in population experiencing a barrier, which in turn influences overall immunization coverage levels. This model will help inform donor investment strategy by identifying high-priority new vaccine attributes and pairing them with high-impact target populations.
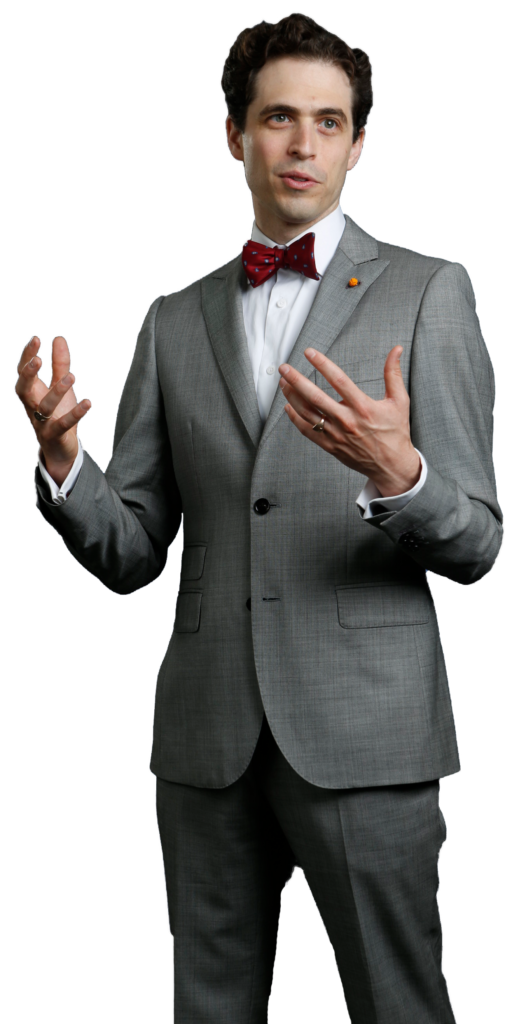
Q & A
with Ari Shwayder
1. What are your favorite types of projects to work on?
There are a bunch of different things I look for in a project, and so my favorite ones are those that combine at least some element from a few of these categories:
2. How is the work you do for WDI different than the work you did while at McKinsey?
It’s a bit hard to say because both McKinsey and WDI do projects in such a broad range of things. I think one of the biggest differences is that at WDI we have fewer resources than a huge consulting firm like McKinsey. You can think of this as a bad thing, but I tend to see it as just meaning that we get to be more choosy about what projects we do and how we’re going to help. We can’t pretend that we’re going to be able to do everything on some massive project. So instead we get to pick the areas where we can have the biggest impact and just go after that. That’s actually quite freeing!
It also means that the mission of WDI is more focused. McKinsey, and other big firms, have a mission to – and are able to – help any large organization with almost any problem. At WDI, we are trying to be more specifically focused on using the tools of economics and market-based thinking to help improve social welfare in low-and middle-income countries. So that gives us a sharper lens through which to pick and tackle our projects.
3. How does your work with WDI inform your other research and project work at Ross?
The biggest area is that it gives me lots of great examples to use in my teaching. I can use situations and examples from WDI to show MBA students how the concepts we’re learning in economics classes really do apply to real-world situations.
I can use situations and examples from WDI to show MBA students how the concepts we’re learning in economics classes really do apply to real-world situations.
Ari Shwayder4. As a Ross faculty member, what is one thing other faculty at Ross might not know about WDI?
I think most faculty don’t have a clear picture of the full scope of things that WDI does and what sort of projects the WDI teams take on. The projects I’ve seen WDI do (and I’ve only been involved in a small percent of them) cover a huge range of topics and would be interesting to lots of different faculty members. There are definitely aspects in projects from economics, operations, organization, etc.
5. What advice would you give a student interested in working in global health after graduation based on your WDI work?
A couple of things:
Ari Shwayder is a research fellow in WDI’s Healthcare Initiative where he provides economic insights and support to projects spanning a broad range of topics. His work with WDI staff includes a project for the Madagascar Ministry of Health to analyze and build a financial model for their drug distribution network, consulting with the Aravind Eye Hospital, Lviv Business School and Ihangane Project MAP teams and researching a project using remittances to improve access to working capital in developing countries.
Shwayder also is a lecturer in Business Economics and Public Policy at the University of Michigan’s Ross School of Business. He has previously worked as a consultant for McKinsey & Company, where he worked on consulting and research projects across a wide range of industries.
Studying for her master’s degree in public health, Alison Granger was interested in a course at the University of Michigan that would let her take the lessons from her textbooks and classroom lectures and put it into practice.
That’s why she enrolled in BA685: Healthcare Delivery in Emerging Markets, a course offered at the Ross School of Business.
“I was interested in getting a more in-the-field, global perspective on what I’ve learned so far in class,” said Granger, who traveled to Ethiopia for her project. “And I did with this class.”
The class is comprised mostly of MBA2 students, but also is open others pursuing other graduate degrees such as Granger. It’s designed to enhance participants’ international leadership capabilities, increase awareness of diverse business issues within the current global landscape, provide on-the-ground experience in a foreign country and contribute to the success of partner health clinics and hospitals. It is taught by WDI President Paul Clyde.
The course, organized and primarily funded by WDI with some financial support from Michigan Ross, responds to the increasing need for managers with international business perspectives to augment their business and management knowledge. During the first part of the term, students learned about healthcare in emerging markets through lectures, guest speakers and case discussions. Students were then divided into five teams and prepared for visits to their selected country, traveling to those destinations in late February and early March.
This year, student teams worked in Ethiopia, India, Kenya, Peru and Rwanda. All five teams presented recaps of their projects on April 22 at Michigan Ross.
Clyde said the travel-study course lets students combine what they learned in the classroom with hands-on experience in the field. It features a collaborative learning environment with faculty and students learning from each other in an action-based learning setting.
“Through this course teams of students from Ross, SPH and School of Information have provided our partner healthcare organizations value through analysis of their operations, customers and strategy,” Clyde said. “Through this experience, the students gain unusual insights into the opportunities and challenges of operating healthcare organizations in LMICs.”
Here is a recap of the BA685 projects:
More than 1 million infants die each year due to severe respiratory distress, with 99 percent of these deaths in low- to middle-income countries, according to the World Health Organization. Current noninvasive ventilators are expensive, require skilled operators, and fail during power outages that are common in emerging markets. AIM Tech developed NeoVent, a low-cost, low-tech, easy-to-use ventilator that is non-electric and has only one moving part. It also can be manufactured at scale for less than 1 percent the cost of conventional ventilators.
 AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
AIM Tech wanted the BA685 student team to evaluate if AIM Tech should enter the Indian market and provide recommendations for a market entry strategy. The students visited Delhi,
Mumbai and Chennai, and interviewed and provided product demonstrations to 24 healthcare facilities, one government official, two manufacturers and one distributor. The students found that the Indian healthcare market shows a high-growth trajectory. The government’s focus on entrepreneurship, insurance, and neonatology also creates favorable climate and demand for NeoVent, while clinicians see the product as unique, necessary and value it at a higher-than-planned price, the students noted.
They recommended AIM Tech license NeoVent to a multinational corporation with an existing foothold in the Indian market. Another suggestion was to pilot NeoVent with a large hospital following FDA approval.
 The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
The lack of reliable, local liquid oxygen suppliers in Ethiopia for hospitals makes it necessary to have an oxygen separator system on the grounds for the hospital EADG is building. EADG asked the BA 685 students to study two questions: should EADG’s future hospital build and operate a medical gas plant?: and, should EADG sell excess medical gas to area hospitals?
Based on research and interviews with hospitals with its own medical gas plants on-site, the students’ findings showed that EADG would benefit from building its own facility and could learn from other hospitals that have done the same. On the question of whether to sell excess medical gas, the students’ research showed it would not be a good decision to do so. It is not profitable, the research found, and there is robust competition and several barriers to entry in the market. The students encouraged EADG to begin the bidding process soon to select equipment suppliers because the hospital is expected to open in 2021. They also suggested EADG monitor the medical gas market for any movement or changes in government policy that might make it more profitable to sell excess medical gas.
Timely and accurate data reports are vital to operations at rural health clinics. Electronic records have been implemented, but poor staffing and internet connection have made e-records ineffective. The Ihangane Project, in partnership with nurses from rural health centers, created E-Heza Digital Health Record to deliver more timely and accurate data to the Rwanda Ministry of Health. The ministry has requested that E-Heza be expanded throughout Rwanda to serve maternal child care.
 The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The BA 685 students project was to establish a framework for evaluating the efficiency of the current data reporting system and E-Heza in terms of timeliness, cost and data quality. To accomplish this, the students: analyzed the current lead time for data to move from point of care to the Ministry of Health; identified the cost of data reporting, including revenue loss; defined measurements to evaluate data accuracy; and developed framework to evaluate the efficiency of data reporting.
The students recommended a framework that evaluated efficiency in terms of timeliness, cost savings and data quality.
For next steps, the students recommended recording observational data for each process in the workflow, testing the framework for E-Heza and other health modules and exploring and quantifying the potential adverse effect due to poor data quality.
The Kisii Eye Care Institute started in 2013 and it has grown from an eye care service provider to a medical eye hospital and training center. It provides 3,000 surgeries annually but wants to increase the demand and capacity to 5,000 per year. Kisii operates as a social enterprise using an entrepreneurial approach to solve a social problem – avoidable blindness and visual impairment. Services are provided at normal rates for those who can afford them and substantially below cost to low-income members of their community.
 The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
The BA685 student team put together a business plan for Kisii to increase demand for its services and improve operational efficiency. The students said surgery and optical services (glasses) are the largest revenue generators for Kisii and it must enhance its marketing strategy in both areas. Operationally, to decrease wait times and provide patients with a higher quality overall experience, current processes must be improved by standardizing the patient queue and improving counselor training, among other things. And to be ready for future growth, the current Kisii organizational structure must change, roles need to be redefined roles and responsibilities shifted.
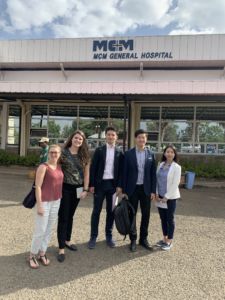
PAMS Policlinico wants to become a gastrointestinal (GI) center of excellence. It currently offers GI services and recently a GI doctor from the University of Michigan visited to develop an operational understanding.
 Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
Last year’s BA685 team conducted a market analysis to determine how PAMS could grow to become a center of excellence in either GI or ophthalmology. This year’s student team built on that previous work and developed a complete business plan that: evaluated marketing strategy; studied GI equipment options to ensure there is an adequate plan for maintenance, repairs and acquisition; and, assessed opportunities to decouple skills and create a new position to take on some of the current physician duties. This business plan will be presented to potential PAMS funders this spring.
The students’ research and on-site observations and interviews showed: A lack of standardized practices lead to operational inefficiencies and lowered capacity even with sufficient personnel; contract incentives are not structured to achieve best outcome for PAMS; omission of certain accounting practice lowers visibility into financial health of PAMS and each specialties; and, the Polyclinic is one of the few providers of colonoscopies in the region.
The student team’s recommendations included: optimizing processes allowing for maximizing use of resources, including supplies and the time of healthcare providers; standardizing processes also decreases waste and allows more patients to be treated per week, ultimately increasing patient volume and with it, revenue.

A 2018 WDI MAP team in Ghana.
Carrie Boyle, a MBA student at Michigan’s Ross School of Business, hopes to work in philanthropy somewhere in the U.S. after graduation. But for a couple of weeks in March, she is excited to be traveling to India as part of the school’s annual Multidisciplinary Action Projects (MAP).
“Working in another country is something I may never get the chance to do again,” she said. “This will be my first time in India and the country really interests me.”
Boyle and her teammates will work with Michigan Academy for the Development of Entrepreneurs (MADE), a nonprofit institute established at Ross by the Zell Lurie Institute for Entrepreneurial Studies, in partnership with WDI and Aparajitha Foundations. MADE works with entrepreneurship development organizations in India to help entrepreneurs operating small- and medium-sized enterprises (SMEs) succeed.
Boyle said she had some criteria when looking for MAPs that interested her.
“I wanted an opportunity to be on the ground having meaningful conversations with the people most immediately impacted by SMEs,” she said. “SMEs employ so many people and impact so many lives.”
Her teammate Shoko Wadano said she too is interested in working with SMEs, “which are very common in India.”
“I’m interested in how businesses mature in India,” she said. “I want to learn what pressures and impacts SMEs have in common, and what kind of value we can bring to them.”
WDI is sponsoring the MADE MAP project along with 10 others this year. MAP is an action-based learning course in which MBA students receive guidance from faculty advisors from WDI and Ross. Each project requires analytical rigor, critical thinking and teamwork. (Find out more about WDI’s MAP projects over the years here.)
After learning about their projects and conducting secondary research for several weeks, the student teams spend two to four weeks working with their organizations in the field.

David Butz
“The complementarities between the talents our students bring and what our sponsors need are sublime,” said David Butz, a WDI senior research fellow in the Healthcare sector who is an advisor on two projects. “Our students experience impact in brand new ways. Our sponsors learn, too, how disciplined management methods can yield dramatic innovations.”
Butz said he enjoys working with the student teams on MAP because it “poses such a unique challenge for both the students and their sponsor organizations, and forces us all to think big.”
“For me, the best achievements are tangible, direct and narrow but at the same time big and high-impact,” he said. “In our short time, can we help to break some key bottleneck, expedite a critical process pathway or otherwise liberate resources and expand capacity? Is the innovation scalable or replicable elsewhere? Do the students and organizations thereby feel empowered?”
Here is a summary of each WDI-sponsored MAP project:
Aravind Eye Care System – India
MAP Team: Rohan Dash, Sid Mahajan, Aman Rangan, Nik Royce
Aravind Eye Care System (AECS) is a vast network of hospitals, clinics, community outreach efforts, factories, and research and training institutes in south India that has treated more than 32 million patients and has performed 4 million surgeries since its 1976 founding.
AECS opened a tertiary eye care center in Chennai in September 2017 that will ultimately serve more patients than any other facility in the AECS system. The MAP team will formulate a detailed three-year strategic plan for Aravind Eye Hospital in Chennai.
CURE International, Inc. – Kenya, Ethiopia, Zambia, Uganda
MAP Team: Dominique James, Sarah Raney, Hannah Viertel, Olga Vilner Gor
CURE operates clubfoot clinics in 17 countries around the world, each tasked with helping children and families deal with the congenital deformity that twists the foot, making it difficult or impossible to walk.
For CURE, the student team will develop a strategic evaluation framework to assess opportunities for market entry and expansion building on global data.
Ghana Emergency Medicine Collaborative – Ghana
MAP Team: Benjamin Desmond, Benjamin Quam, Nicholas Springmann, Vishnu Suresh
The Ghana Emergency Medicine Collaborative aims to improve emergency medical care in Ghana through innovative and sustainable training programs for physician, nursing and medical students. The goal of the training programs is to increase the number of qualified emergency health care workers retained over time in areas where they are most needed.
The MBA team will formulate a detailed strategy to implement interoperable digital payment systems in Ghanian hospital emergency departments.
India Investment Fund – India
The India Investment Fund is working to become the first international, student-run fund at the Ross School of Business. Ross MBA students would be responsible for investing, managing and growing a real investment portfolio.
MAP Team: Charlie Manzoni, Patrick Riley, Queenie Shan, Sheetal Singh
The student team will conduct due diligence on Indian small- and medium-sized enterprises to assess viability for investments, and an appropriate financing instrument.
Infra Group – Ethiopia
MAP Team: Rin Chou, Chandler Greene, Yuki Ito, Brittany Minor
Infra Group is diversified international group with business units in financial services, industries and infrastructure development. Infra Group helps build a more prosperous society through global-scale business development with integrity as its top priority.
The MAP team will conduct due diligence on a group of small- and medium-sized enterprises (SMEs), and recommend which ones to invest in and what amount to invest.
Lviv Business School & Ukranian Catholic University – Ukraine
MAP Team: Blake Cao, Emily Fletcher, Kelsey Pace, Adam Sitts
Lviv Business School and Ukranian Catholic University is a private educational and research institution in western Ukraine.
The student team will undertake a needs assessment of the small- and medium-sized enterprises (SMEs) to determine if Lviv Business School should begin offering consulting services to these SMEs and if so, how those should be structured.
MADE – Poornatha/Aparajitha Foundations – India
MAP Team: Carrie Boyle, Lawrence Chen, Dillon Cory, Shoko Wadano
Michigan Academy for the Development of Entrepreneurs (MADE) is a nonprofit institute established at the Ross School of Business by the Zell Lurie Institute for Entrepreneurial Studies, in partnership with WDI and Aparajitha Foundations. MADE works with entrepreneurship development organizations in developing countries to give individuals operating businesses in these environments the knowledge and best practices they need to thrive.
The MAP team will develop an expansion plan for MADE in the southern Indian state of Tamil Nadu.
The Ihangane Project – Rwanda
MAP Team: Lauren Baum, Nadia Kapper, Paul Mancheski, Jason Yu
The Ihangane Project (TIP) empowers local communities to develop sustainable, effective, and patient-centered health care delivery systems that holistically respond to the needs of vulnerable populations. Partnering with Ruli District Hospital and its associated health centers, TIP is working to identify key strategies for improving health outcomes.
The student team will develop a business model to grow the ready-to-use therapeutic food that is used to treat severe, acute malnutrition.
WEEKEND MBA MAP PROJECTS
Awash Bank – Ethiopia
MAP Team: Matthew Campbell, Joshua Dodson, Joseph McCarty, Aman Suri
Awash Bank, a private, commercial bank, was established in 1995 and features more than 375 branches across the country.
The MAP team will develop a product that can provide capital to small- and medium-sized enterprises (SMEs) in Ethiopia by utilizing remittances already being sent back to that country. The students will work with the bank on all aspects of the loan product. They also will give the bank recommendations on how to monitor the loan and provide business support to SMEs that borrow from the fund.
Grace Care Center – Sri Lanka
MAP Team: Daniel Cady, Yizhou Jiang, Gerardo Martinez, Daniel Murray
The Grace Care Center (GCC) is a home to about 70 orphaned children that offers daycare services and vocational training. It also is home to several poor and displaced seniors, many of whom have chronic health issues such as hypertension and diabetes.
Past MAP student teams from the Ross School of Business developed a diabetic care center model for GCC. This year’s student team will examine the current model and make any needed updates and revisions.
International Clinical Labs – Ethiopia
MAP Team: Emily Mascarenas, Torre Palermino, Alexander Santini, Matthew Traitses
ICL was established in 2004 to provide quality laboratory service all over Ethiopia. ICL serves more than 240 health care centers throughout the country, and is expanding its service throughout Ethiopia.
The Ethiopian government is building its first medical waste incinerator facility outside the capital city of Addis Ababa and has committed to building seven more around the country. WDI is assisting a group of business managers with business plan advice who are interested in managing the business aspects of operating the incinerators. The MAP team will develop a proposal to be presented to the government later this year for the business managers to operate the incinerators.
Sally Stephens, the Feb. 12 WDI Global Impact Speaker and chief business officer of Medicines360, the only nonprofit pharmaceutical company with a marketed product in the U.S., sat down for a one-on-one interview while on campus. (Watch the interview below.)
Stephens was interviewed by Andrea Bare, senior advisor with WDI’s Healthcare focus area, who talked with Stephens about a number of the organization’s operations. Stephens detailed Medicines360’s origin, its business model and how it operates, its approach to partnerships, how the U.S. market compares to sub-Saharan Africa and what the future holds.
Regarding partnerships, Stephens told Bare that Medicines360’s approach is to “partner if someone has the expertise that will help us meet our mission,” she said. “We saw a lack of expertise in the U.S. public sector, so we developed that expertise.”
She said the same “myths and gaps” exist in both the U.S. and sub-Saharan Africa markets. For the future, Stephens said, Medicines360 will “focus on broadening our impact.”
“It is all about access for us,” she said.
Medicines360 has a unique mission-driven business model and an innovative partnership with Allergan. As its name implies, Medicines360 has a global focus and is driven to meet an unmet need for women around the world, including in the U.S. That is, affordable, long-acting contraceptives.
Its first product is a hormonal intrauterine device, or IUD, which had been out of reach for many women because of the high cost of the sole brand on the market. Medicines360 offers its FDA-approved Liletta at a discounted price to public sector clinics across the U.S. to increase access to this important family-planning product.
Additionally, Medicines360 has been working with international health organizations to offer the product, branded as Avibela in low- and middle-income countries, to also increase access to these markets. Avibela was launched in Madagascar in 2018. Sales of Liletta in the U.S. help fund research and development efforts by the company to bring contraceptives to countries such as Madagascar.
Stephens, who joined Medicines360 in 2011, leads the corporate strategy, business development, marketing and sales, and the developing countries programs at the organization.
This article reviews the changes that have taken place in health care delivery in low- and middle-income countries since 1992 and highlights the role of the private sector. It looks at changes in causes of death and also provides an in-depth view of areas likely to take on more prominence and/or change health care delivery in the future.